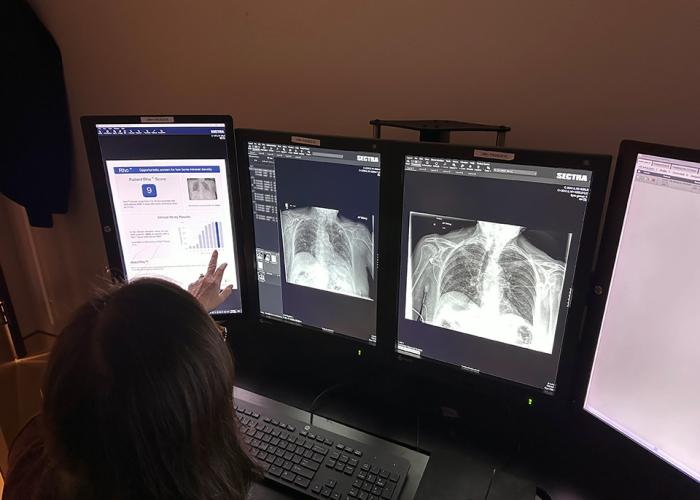
CMH's future is very bright. By 2024, its extensive and comprehensive construction project will be finished making it the most modern hospital within the region. At that time, CMH will see unprecedented growth in all major services, including surgery, medicine and diagnostic imaging. It is also a proud founding member of the Cambridge North Dumfries Ontario Health Team that looks to transform health for our communities.

Our Roots
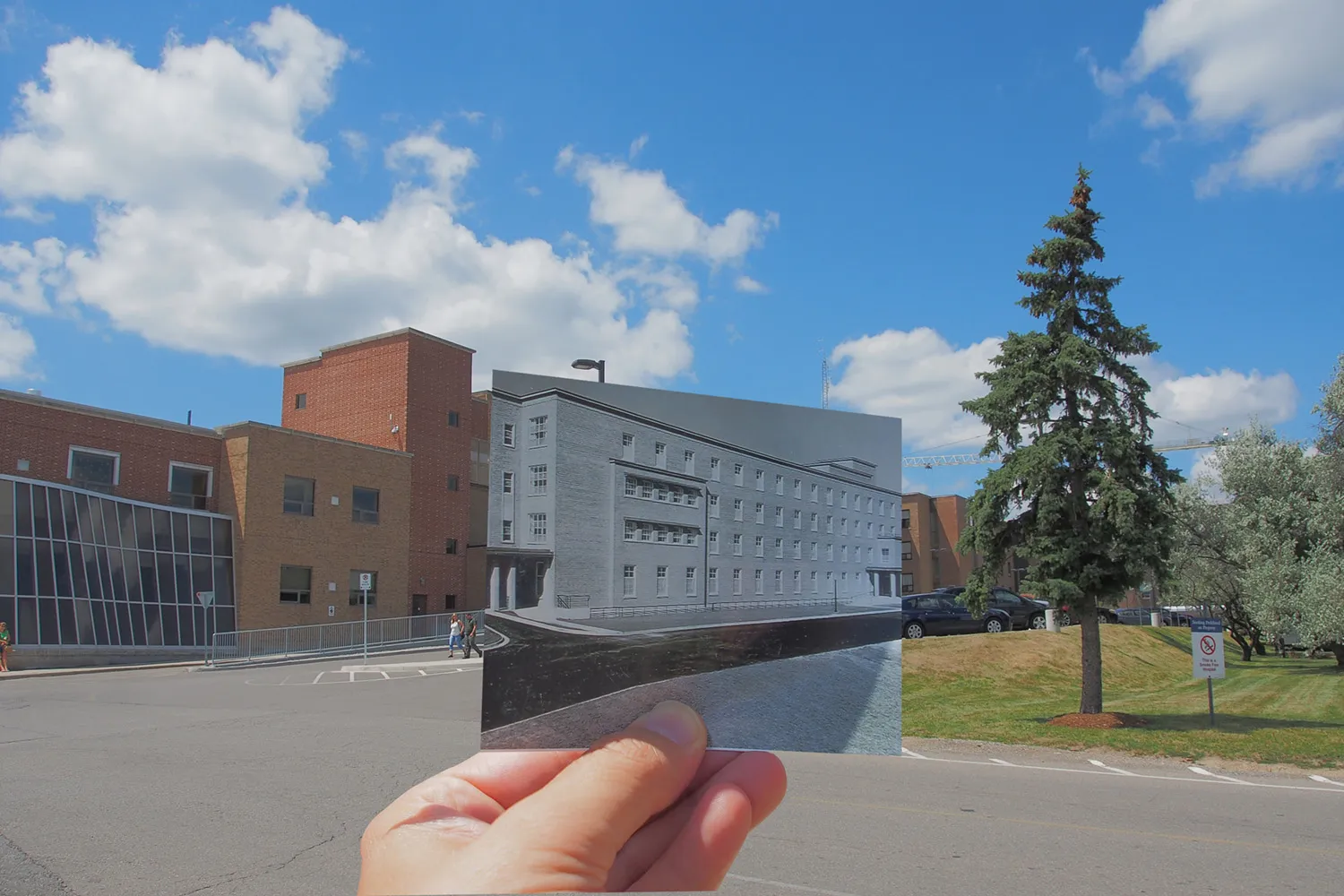
Cambridge Memorial Hospital proudly traces its roots to 1888, when the Region of Waterloo’s first community hospital, known then as Galt Hospital, opened its doors to treat patients in a localized health care setting.
Sixty-five years later, in 1953, a brand new facility was built on the current Coronation Blvd. location, which was better suited to serve the major communities of Galt, Hespeler, Preston and the Township of North Dumfries. At that time, the hospital was also renamed South Waterloo Memorial Hospital in honour of the local women and men that gave their lives for their country. As local boundaries changed and communities merged to become the City of Cambridge, the hospital adopted the new name of Cambridge Memorial Hospital. Prior to 2014, the last major expansion of the hospital was in the early 1970's when the Wing B patient care facility was built.
In 2020, a new patient care wing was opened, that featured the latest building hospital building codes and technologies to help keep staff and patients safe. With the timing of COVID-19 coming to the region a few months later, these safeguards proved invaluable to keeping outbreaks at a minimum during the pandemic. Once the 50-year old Wing B refurbishment is finished, it will boast the same advanced technologies and safety features as Wing A.